Abstract
Background: Drug resistance and non-healing bone damage are the primary causes of morbidity and mortality in multiple myeloma (MM). Proteasome inhibitors (PIs), a mainstay of MM therapy, inhibit cancer growth and are bone anabolic, but drug-resistant relapses negate their benefit. Sphingolipid dysregulation confers PI resistance. Sphingosine 1-phosphate analog, fingolimod (FTY720), improves bone health in multiple sclerosis and is well-tolerated long-term. High doses of fingolimod directly inhibit the in vitro growth of multiple cancers but these doses may not be clinically achievable. The combination has not been developed as a myeloma treatment.
Method: We explored the effects of fingolimod alone and in combination with bortezomib on tumor growth and osteoblastic differentiation in vitro, in ex vivo co-culture of human MM cells and mouse bones, and in xenograft models.
Results: Fingolimod IC50s for growth inhibition of human MM cell lines and primary MM cells are 3-6 uM, at which dose is toxic to primary osteoblasts, osteocytes, osteoclasts and bone explants. Fingolimod at doses between 10-100 uM, similar to blood levels seen in MS patients, had no effect on the growth of MM cells and bone cells. At these doses, fingolimod increased alkaline phosphatase, and osteocalcin mRNA promoted nodular calcification of primary pre-osteoblasts, suggesting its ability to promote osteoblastic differentiation. In addition, fingolimod (10-100 nM) + bortezomib (3 nM) promoted nodular calcification of pre-osteoblasts, compared to each drug alone.
In mouse bone explants, fingolimod not only increased alkaline phosphatase and osteocalcin mRNA, but also inhibited osteoclast (evidenced by acid phosphatase (ACP5) and cathepsin K mRNA downregulation), and promoted osteocyte differentiation (evidenced by an increased osteocyte-gene DMP1), all of which supported its multifaceted bone anabolic effects. When human MM cell lines were cultured with mouse bone explants, MM cells engrafted on mouse bones and induce osteolytic lesions. One-week 100 nM fingolimod treatment had a limited effect on tumor growth. Fingolimod + bortezomib (3 nM) inhibited tumor growth more significantly than bortezomib alone (p<0.05). Tumor-colonized bones showed increased ACP5 and cathepsin K, evidence of osteoclast activation, of which levels were significantly more inhibited by fingolimod and bortezomib combination than each agent alone. In addition, fingolimod significantly enhanced osteocalcin and DMP1, while bortezomib showed minimal effect on these gene expression levels. In comparison, zoledronic acid, a currently approved agent in MM bone disease only inhibited acid phosphatase and cathepsin K, and had no effect on MM growth.
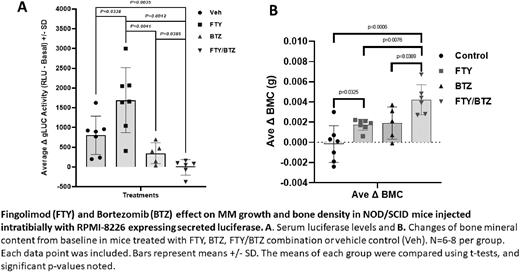
The benefit of the combination was further tested in xenografts of NOD-SCID mice intratibially injected with the secreted luciferase-expressing RPMI-8226 cells. In this model, MM cells were engrafted locally in the injected tibia. Contralateral tibiae served as controls. Spines represented distant sites for systemic effects of MM-mediated soluble factors. Four weeks after injection, mice were randomized based on serum luciferase activity- a measurement of tumor burden, to the 2-week treatment of fingolimod (i.p. 5 mg/kg) 3x/wk), bortezomib (s.c. 0.25 mg/kg) 2x/wk), the combination or vehicle controls.
Fingolimod showed no effect on tumor growth. The combination inhibited MM growth more significantly than bortezomib alone (Fig. A). In the tumor-injected tibiae, bone mineral density was significantly increased by the combination, more than fingolimod or bortezomib single agent (Fig. B). An increase in the vertebral bone mineral density was only observed with the combination treatment.
Conclusions: Fingolimod at a clinically relevant dose synergizes with bortezomib to inhibit MM growth in the bones, likely via an indirect effect on the bone marrow microenvironment rather than direct cytotoxicity. In addition, fingolimod has synergistic bone anabolic effects when combined with bortezomib. The two effects may be related. Work is ongoing to validate the combination in patient-derived xenografts (PDXs) and to develop a risk model based on the sphingolipid gene signature of primary MM cells to define a patient subset likely to benefit from the combination to facilitate future clinical trial.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal